Get 40 Hours Free Developer Trial
Test Our Developers for 40 Hours at No Cost - Start Your Free Trial →
Did you know that 95% of USA healthcare providers rely on HL7 standards to share data? Medical organizations now see HL7 integration as key to improving data sharing and making their operations smoother in today’s healthcare system.
Every year, a single patient produces nearly 80 megabytes of medical records and imaging data. This leads to an increasing pile of healthcare data that must be shared and organized. This data challenge highlights why most healthcare leaders see health data interoperability as their top concern. Over half of healthcare groups also aim to spend more on global health data interoperability projects every year.
HL7 helps healthcare systems work together by linking software solutions from different healthcare vendors through common protocols. Health Level Seven, or HL7, was founded in 1987 as a nonprofit group. It offers the structure needed to let your systems exchange information, no matter their vendor or setup.
This article explains why HL7 integration matters to your healthcare system, how it works in real-life practice, and highlights the benefits it offers.
Quick Snapshot
If you’re short on time, here’s the quick version:
| Challenge | HL7 Integration Fix |
|---|---|
| Data silos between EHR/RIS/LIS | Unified data exchange |
| Slow clinical decisions | Real-time messaging (cut decision time ~14 min) |
| Heavy admin workload | Up to 30% task reduction |
| Compliance complexity | Simplifies HIPAA reporting |
| Duplicate tests | Prevents costly repeat procedures |
| Telehealth/AI scaling | FHIR-ready APIs |
What is HL7? Why It Matters in Healthcare?
Understanding HL7 and Health Level Seven
People often call Health Level Seven by its short name HL7. It includes a set of global rules meant to share clinical and administrative health information between software. HL7 International, a nonprofit organization formed in 1987, works to develop systems that enable healthcare platforms to share data effectively. The name “Level Seven” points to the application layer, which is the seventh layer in the Open Systems Interconnection (OSI) model. This model provides a structured way to organize communication tasks.
HL7 International focuses on a clear goal: to let people access and use the right health data whenever and wherever needed. This group plays a key role in improving how healthcare data moves between platforms and providers.
HL7 standards and their purpose
HL7 standards offer guidelines to manage how healthcare data is shared and stored. They explain the way information needs to be formatted and transferred, covering details like data structures, types, and communication methods.
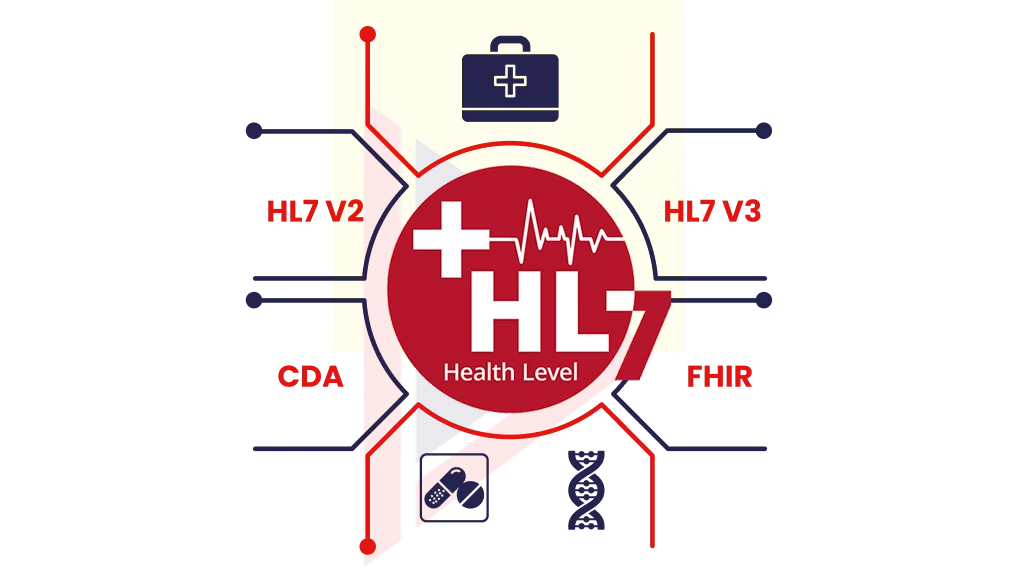
There are different versions of HL7 standards, each designed to meet specific requirements:
- HL7 V2.x is the most used version, relied on by 95% of US healthcare organizations and adopted in 35 countries.
- HL7 V3 works as a standard for Electronic Health Records and is used by governments and agencies.
- Clinical Document Architecture (CDA) sets rules for clinical documentation.
- Fast Healthcare Interoperability Resources (FHIR) blends past features with modern web tech in a newer API-based framework.
These standards aim to make sure data is shared in a uniform way and maintain consistency between systems, even when the systems come from separate healthcare groups.
Role of HL7 in healthcare
Healthcare today relies on systems exchanging and linking data. Interoperability is key to making this possible. Standards like HL7 play a key role because implementing EHR depends on them.
HL7 plays a key role in healthcare interoperability. It:
- Allows patient information to move between different systems
- Helps hospitals, clinics, and labs share information using common standards
- Maintains consistent and accurate data across various platforms
- Cuts down on extra paperwork by automating processes
The impact goes beyond just transferring data. A study revealed that using HL7 standards results in a reduction in “patient journey time” by over 14 minutes and cuts “time to identify” patients by 10 minutes. These time savings lead to better care for patients and smoother operations overall.
Healthcare organizations across the globe use HL7 integration to build the backbone of their communication systems. Without HL7’s standard protocols, healthcare systems would struggle with fragmented communication and create significant barriers in sharing information.
Top 6 Reasons Your Healthcare System Needs HL7 Integration
Healthcare systems today deal with growing demands to provide seamless and effective patient care. Implementing HL7 offers 6 strong benefits that tackle these issues head-on.
Better connection between EHR, RIS, and LIS systems
The most important benefit of HL7 integration lies in improving how different healthcare systems work together. HL7 acts like a common language that helps Electronic Health Record systems, Radiology Information Systems, Laboratory Information Systems, and other tools share information. This setup creates more consistent and standardized data across systems. It also breaks down barriers that often block smooth and connected patient care.
Using set methods to share data, healthcare groups get a fuller picture of patient details. This broader understanding helps them make smarter choices and provide better care throughout the whole organization.
Regulatory compliance with HIPAA and HL7 standards
HL7 is key to ensuring compliance with regulations. HIPAA and HL7 demand reliable security measures like encrypting data, controlling access, and keeping audit records to safeguard private patient details.
Health Level 7 integration lets healthcare providers send data to regulators through electronic systems. This helps organizations follow public health reporting rules without trouble. Making compliance simpler cuts down on paperwork and lets healthcare teams spend more time improving patient care instead of dealing with tricky compliance processes.
Faster clinical decision-making with real-time HL7 data
Getting full patient info has a big impact on making better clinical decisions. More than anything, real-time HL7 integration allows faster sharing of clinical details. This helps doctors decide faster, improve how treatments work, and reduce illness risks.
For example, when a hospital’s EHR system uses HL7 messaging to add lab test results, doctors can spot issues like uncontrolled diabetes in patients and set up needed follow-up visits. HL7’s real-time data sharing also gives instant alerts about unusual test results or vital signs, helping doctors react sooner to possible health problems.
Automated workflows and reduced manual work
HL7 makes workflows easier by bringing in automation. It uses standard methods to share data, which cuts down on the need to enter information by hand. This boosts productivity and helps systems run more efficiently.
Healthcare organizations that use HL7 standards see a boost in workflow efficiency and fewer mistakes because automated systems take over manual tasks. Automation saves time, allowing workers to focus on important duties like patient care and workforce planning. Some report cutting their administrative tasks by as much as 30% with these solutions in place.
Cost savings through test and procedure deduplication
It allows smoother data sharing, which helps reduce expenses. Providers with full access to patient records can skip doing duplicate tests or procedures.
For instance, when a patient’s lab results come through HL7 messages, a doctor can rely on those instead of requesting more tests. This method helps cut healthcare costs and avoids putting patients through extra procedures that carry risks.
Also Read: How Much Does It Cost to Develop Healthcare Software?
Support for AI, Telehealth, and HL7 FHIR integration
Health Level 7 offers essential backing to growing technologies. HL7 International set up an AI Office to create rules to ensure AI in healthcare stays safe and reliable, aiming to bring better health results for everyone.
To support telehealth applications, HL7 FHIR makes data sharing easier by designing resources such as patient observation, medication, and appointment to allow instant communication in virtual consultations. This standard helps healthcare workers get important patient details faster while using telehealth services.
FHIR uses a modular setup that helps telehealth systems expand while keeping performance steady. This approach paves the way to improve how healthcare is delivered. By using FHIR-powered tools, healthcare groups get access to AI features, detailed analytics, and mobile apps that make patient care and involvement better.
Understanding HL7 Standards and Message Types
To implement HL7 in healthcare systems, you need to understand its standards and message formats. Having more detailed knowledge of the various HL7 versions, message types, and data structures helps you build strong interoperability solutions.
Overview of HL7 V2 V3, CDA, and HL7 FHIR
The HL7 family includes different standards that have developed over the years to fit the evolving needs of healthcare.
HL7 V2 serves as the foundation of healthcare communication. It remains the primary standard in 95% of US healthcare systems. People often describe it as the “workhorse of electronic data exchange.” It relies on a message-based system that uses delimited text to format information. Even though it first appeared in the 1980s, its straightforward design and reliability keep it in use.
HL7 V3 appeared in the early 2000s, introducing a structured method rooted in the Reference Information Model (RIM). It relies on XML messaging to boost data consistency. But its complexity has restricted its use to healthcare IT projects led by governments.
The Clinical Document Architecture, or CDA, is HL7’s most-used V3 standard. It includes a standard header with metadata and allows sharing clinical details in different formats. Its XML-based design makes it great for exchanging documents.
Fast Healthcare Interoperability Resources (FHIR), which appeared in 2014, is the latest standard. It builds on earlier versions by merging their strengths with modern web tools. FHIR works better than older standards because it relies on resources. These are modular pieces that represent ideas like medications or patients. It also supports various formats such as JSON and XML.
Common HL7 message types: ADT, ORM, ORU, SIU
Different healthcare systems share data by using specific message types, with each having its own purpose:
- ADT (Admission, Discharge Transfer): Systems use this message type the most. It deals with patient movement and demographic info using segments like PID for patient identification and PV1 for their visit details.
- ORM (Order Message): Systems share details about orders through this. It covers things like prescriptions, lab work, or treatments.
- ORU (Observation Result): This sends clinical observation details. It includes lab results, vital signs, and other patient-related data.
- SIU (Scheduling Information Unsolicited): This one handles appointment scheduling. It allows recording, updating, or canceling with 14 unique trigger types.
Real-world events like admitting a patient, receiving test results, or scheduling an appointment set off each message type, starting the sharing of standardized details.
HL7 data types: ST, NM, TS, CE, XCN
HL7 messages include fields that use specific data types to control the type of data they hold:
- ST (String Data): Contains simple text
- NM (Numeric): Holds numbers
- TS (Timestamp): Stores dates and times
- CE (Coded Element): Has codes along with their meanings
- XCN (Extended Composite ID and Name): Combines names and identifying codes for people
These data types bring structure and make messages consistent so systems receiving them can interpret. More advanced data types include parts or smaller pieces that relate to other data types.
Knowing these standards, message kinds, and data setups builds the base to succeed in HL7 integration projects. This lets healthcare systems share information.
How HL7 Works in Real-World Systems
Healthcare systems rely on various proven methods to make HL7 work. These methods enable clinical systems to share data. Learning about these approaches helps healthcare providers choose the right way to integrate their systems.
Point-to-point vs HL7 integration engine
Healthcare systems usually use two main methods to implement HL7. The point-to-point approach sets up specific interfaces so two systems can share data. HL7 makes it easier to understand the data format between those systems. But when more systems are added, it can get messy. Adding a new system means creating several more interfaces, which complicates things and raises maintenance expenses.
HL7 engines act as middleware to link several systems at once. These tools convert data formats to meet the unique needs of each system and manage how messages move through workflows. By removing the need for several point-to-point system links, integration engines cut down both costs and the time needed to set up. Well-known tools in this space include Infor Cloverleaf, Healthshare Ensemble, Core Health Corepoint, and NextGen Connect (Mirth Connect).
Role of HL7 APIs in modern healthcare
HL7 APIs play a crucial role in sharing healthcare data today. These standard tools let EHR systems communicate with each other, pulling important patient details from various places. They also help telemedicine platforms link with EHR systems. This connection allows doctors to hold online consultations while viewing full patient records.
FHIR uses these API features by standardizing resources to describe clinical ideas such as patients, observations, and medications. FHIR servers act as central hubs that manage how patient data is accessed within healthcare systems.
Sample HL7 message exchange between systems
An HL7 message flow works through a query and response process. One system sends a request, often prompted by a clinical event. This request goes to the integration engine, which converts it into the required HL7 format. The system receiving the request searches its database and creates an HL7 message as a reply. The integration engine then changes this reply into a format the original system can read, wrapping up the communication loop.
This method helps different healthcare systems share data and ensures the information stays consistent during the exchange process.
Why Choose TechnoBrains for HL7 Integration
Choosing the right partner to manage integration plays a big role in making sure your healthcare system works well together. TechnoBrains not only delivers reliable HL7 integration services but also provides end-to-end healthcare software development solutions that enhance data interoperability and workflow efficiency.
Expertise in HL7 FHIR APIs and EMR integration
TechnoBrains provides professional HL7 integration support through a team of certified specialists who have deep knowledge of both older HL7 standards and newer FHIR frameworks. Our developers handle various messaging methods like TCP/MLLP, HTTP, SOAP, and FTP/SFTP to move healthcare data. We also offer FHIR interface solutions, creating clear plans and setting them up on AWS Cloud and Azure Cloud systems.
Custom HL7 interface development and testing
The company specializes in creating custom interfaces to handle different message types:
- Bi-directional interfaces like ADT, SIU, and billing
- Order management (ORM) and result reporting (ORU)
- Clinical documentation and charges
TechnoBrains focuses on thorough testing. They check connectivity, run unit tests, and perform integrated testing with experts to ensure everything works as intended.
End-to-end support from planning to validation
TechnoBrains handles the full integration process from analyzing initial needs to supporting systems after they go live. Their work involves analyzing interfaces in detail, creating proper specifications, running thorough tests, and helping with deployment. They also focus on maintaining and improving current interfaces to ensure systems work at their best.
Conclusion
HL7 integration is a key part of today’s healthcare systems. It connects EHR, RIS, and LIS to make smooth data sharing and clinical decisions faster. With workflow automation, better compliance, and fewer duplicative tests, HL7 both optimizes efficiency and improves the quality of patient care.
As the healthcare landscape progresses, HL7 – particularly new standards, including FHIR – prepares the groundwork for advanced technologies like AI and telehealth. Collaborating with TechnoBrains guarantees a seamless, secure, and scalable HL7 integration, which allows your business to provide more intelligent connected healthcare.
Still have questions? Reach out to TechnoBrains for a smooth HL7 integration or a fully functional healthcare software application that is ready for the future.
HL7 Integration FAQs
HL7 integration helps healthcare systems share accurate data between EHRs, labs, and clinics. It improves teamwork and makes workflows smoother.
HL7 delivers lab results and vital signs that save about 14 minutes per patient during decision-making.
Yes. It stops duplicate tests and avoids unnecessary procedures, saving money for patients and providers.
By using FHIR APIs, telehealth apps pull patient data instantly and support AI-driven analytics for better results.
HL7 V2 uses a basic, message-focused design and feels older. FHIR relies on APIs offering flexibility and scaling for modern apps.
Not always, small clinics handle point-to-point setups. Larger systems need HL7 for scalability.
Yes, it stays within HIPAA guidelines.