Get 40 Hours Free Developer Trial
Test Our Developers for 40 Hours at No Cost - Start Your Free Trial →
Medical coding stands as a vital component supporting healthcare operations and financial sustainability. It achieves its primary function by generating steady billing procedures that enable fast payments. Interruptions in coding can extend claim processing times and lead to rejections.
In today’s healthcare system, coding teams face major difficulties because they experience higher patient numbers and require more detailed medical documentation, and operate under shifting insurance company rules. The shortage of skilled coders further intensifies these pressures. The healthcare industry must use artificial intelligence-based automation because more than 80% of medical bills contain errors, which lead to approximately 42% of claim denials through coding mistakes.
Healthcare organizations relying on traditional manual workflows face three major issues: backlogs, higher denial rates, and delayed payments. Automated solutions help eliminate inefficiencies, improve task efficiency, boost staff output and accuracy, and enhance revenue cycle results without adding extra work.
What is AI Medical Coding?
These services utilize artificial intelligence to enhance and streamline operations involving medical codes derived from clinical documentation. The system enables healthcare providers to convert physician notes, medical diagnoses, and treatment procedures into accurate medical codes with reduced manual work requirements.
This approach is quickly becoming the standard practice across the industry. The healthcare industry experiences steady growth, reflecting the operational difficulties healthcare teams encounter because manual coding systems cannot keep pace with the increasing demand for complex work. Smart coding solutions help providers increase accuracy and decrease claim rejections while they protect their revenue streams.
Unlike traditional medical coding tools, intelligent coding solutions can understand both structured data from electronic health records and unstructured data, such as free-text physician notes. This allows coding teams to work more efficiently while maintaining accuracy and compliance.
These AI-driven coding systems assist coders rather than replace them, reducing repetitive work and letting them focus on complex cases. Hospitality software uses similar AI-driven methods to streamline operations.
How AI Medical Coding Work?
Medical coding scans medical documents to find correct codes through its advanced pattern detection systems, which simultaneously check its compliance with legal requirements and enable human operators to assess the results. The system improves both precision and operational speed through its automated processes, which decrease the need for human work. This system,
- Applies natural language processing to analyze clinical notes and encounter details, which allows it to determine the actual care that was delivered.
- Suggests suitable ICD, CPT, and HCPCS codes by analyzing patterns that it learned from previously approved claims and their coding decisions.
- Enhances its search capabilities through its ability to learn from both past data and coder assessments, which helps it achieve improved accuracy during common case processing.
- Validates codes against compliance rules and payer guidelines before submission, while HL7 integration provides seamless data transmission and early problem identification.
- Human coders perform a review process to modify and authorize final codes, which helps maintain quality control for business operations that need to expand.
Medical Coding with AI Compared to Computer-Assisted Coding
For healthcare providers, moving from computer-assisted coding to advanced automation-based coding is a step toward more accurate coding, fewer denials, and stronger revenue cycle management.
| Aspect | Computer-Assisted Coding | AI Medical Coding |
|---|---|---|
| Core approach | Relies on predefined rules and keyword matching | Uses artificial intelligence to understand clinical context |
| Handling clinical notes | Limited understanding of free-text documentation | Interprets structured and unstructured clinical data |
| Manual effort | Requires heavy manual review by coders | Reduces manual review while keeping human oversight |
| Adaptability | Needs frequent rule updates to stay accurate | Improves over time by learning from data |
| Coding accuracy | Prone to errors when documentation is complex | Delivers more consistent and accurate coding |
| Scalability | Struggles with high chart volumes | Scales well for high-volume healthcare environments |
| Denial reduction | Limited impact on preventing denials | Helps reduce denials through better code validation |
| Impact on the revenue cycle | Offers incremental efficiency gains | Supports stronger revenue cycle management |
Looking to Implement AI Medical Coding Services?
See how TechnoBrains can work for your organisation.
Talk to Our Healthcare AI Experts!
How AI Medical Coding Improves Revenue Cycle Performance?
Advanced automation-based coding solutions improve revenue cycle management by reducing manual effort and increasing accuracy early in the process. This helps healthcare providers get paid faster, minimize errors, and reduce rework across billing and claims workflows.
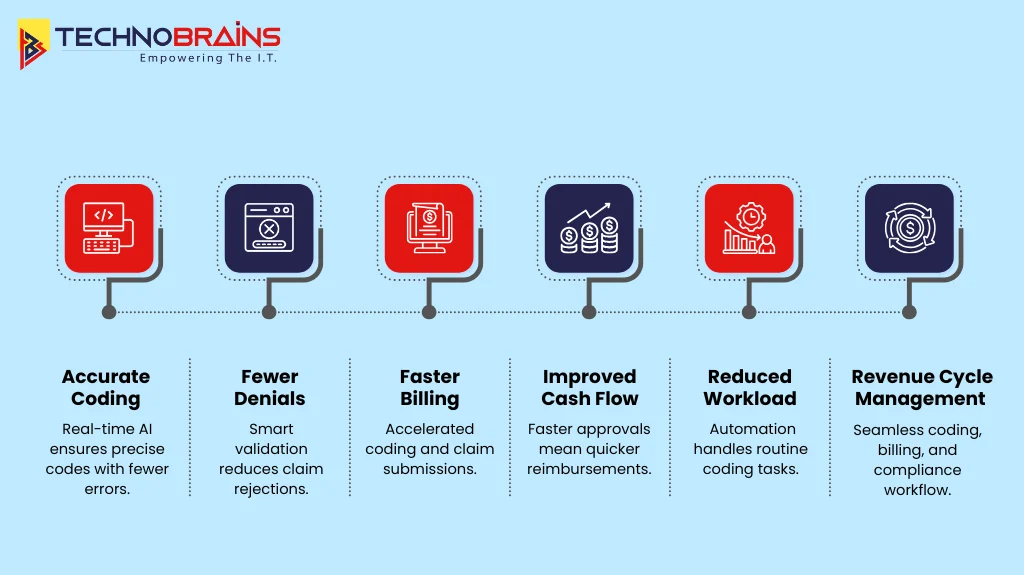
Enhanced Coding Accuracy
Accurate coding forms the foundation of effective revenue cycle operations. Intelligent coding platforms analyze clinical documentation using standardized logic to reduce errors, documentation gaps, and missed modifiers, while medical chatbots capture accurate patient information to improve documentation quality.
Reduction in Claim Denials
A large portion of claim denials stems from incomplete information, together with incorrect code combinations that create major problems. The automated coding systems validate codes through their submission process by using payer-specific rules alongside historical denial patterns to reduce both preventable denials and rework requirements.
Accelerated Billing and Cash Flow
Manual coding methods often cause delays in the billing process, creating obstacles that result in slower reimbursement cycles. The automation tools simplify the charge processing procedure while they speed up claim submission and improve payment processing times without requiring extra staff members or increasing business expenses.
Decreased Operational Burden on Coding Teams
Repetitive administrative tasks frequently cause coding professionals to experience both physical and mental exhaustion, which results in burnout. The automation-driven solutions handle all routine work tasks, which boost productivity and enable coders to focus on their most important responsibilities, which include detailed reviews and audits.
Enhanced Revenue Cycle Visibility
Consistent coding data across charts and claims helps the revenue cycle process achieve better transparency overall. The enhanced visibility allows leadership teams to identify emerging trends while they assess potential risks and make staffing decisions together with audit planning and process optimization decisions.
Core Technologies Behind AI Medical Coding and Billing
AI-driven coding and AI medical billing are powered by a combination of advanced healthcare AI technologies. These systems are designed to understand clinical language, adapt to changing documentation, and integrate smoothly into existing healthcare workflows. Many organizations use AI consulting to implement and optimize these systems efficiently.
Natural Language Processing in Medical Coding
Natural language processing enables AI systems to process unstructured clinical notes, which contain information about medical diagnoses and treatment procedures and contextual details that clinicians have recorded. The process results in better accuracy and needs less manual effort to complete.
Machine Learning in Healthcare Coding
In today’s world, machine learning enables AI systems to learn from previous claim data, denial records, and coding information, which allows them to improve their accuracy over time while effectively managing difficult cases.
EHR Integration and Workflow Compatibility
The platform achieves seamless EHR integration, which enables artificial intelligence systems to obtain access to clinical records and billing information and return codes while maintaining existing operational procedures. The system uses this approach to decrease the need for human data entry work, which leads to more efficient coding operations.
HIPAA Compliant AI for Healthcare
A HIPAA-compliant AI protects patient data through secure handling methods, which establish role-based access and maintain audit logs while providing compliance support and automated system scalability.
From Medical Coding Automation to Autonomous Medical Coding
In today’s world, automation handles routine coding tasks while human workers dedicate their time to conducting reviews and audits and managing complex cases, which results in improved operational efficiency and maintains effective oversight and compliance with regulations.
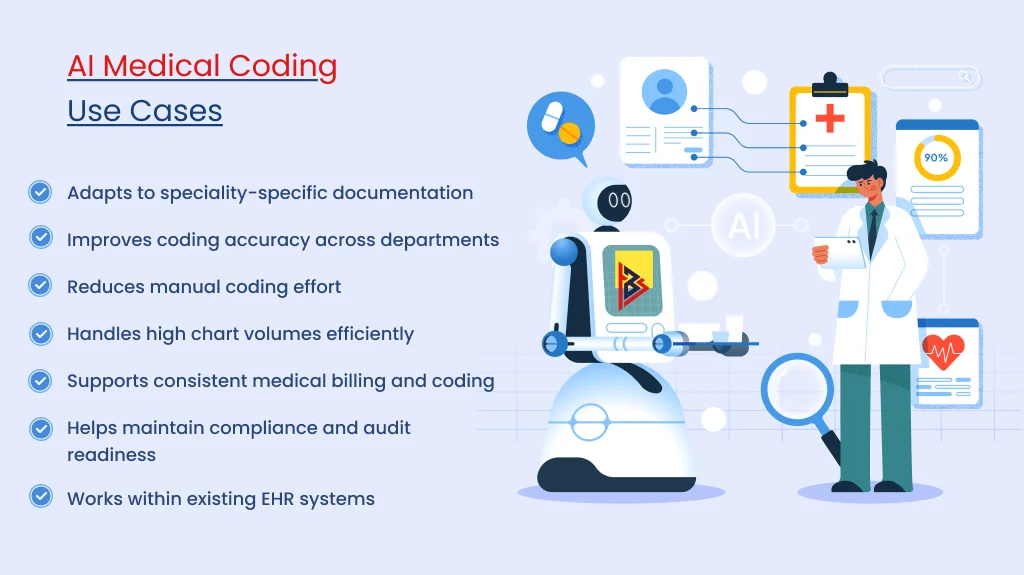
AI Medical Coding Use Cases by Healthcare Specialty
How Automated Medical Coding Supports Different Healthcare Specialties?
AI medical billing is not one-size-fits-all. Different specialities face different documentation patterns, coding complexity, and revenue risks. Healthcare AI delivers the most value when applied to the right workflows within each specialty.
Primary Care and Outpatient Clinics
In primary care settings that manage heavy patient traffic, the repetitive nature of services makes them ideal for automated coding systems. AI establishes standardized procedures for normal medical appointments while enabling coders to concentrate on outstanding cases.
- The system automatically generates medical codes for standard patient appointments.
- The system decreases the need for manual work while enhancing the speed of claim processing.
- The system empowers coders through their evaluation of unique medical cases.
Emergency Departments
In emergency departments, unpredictable documentation and time constraints create major challenges. AI analyzes unstructured clinical documentation to extract billable services and enhance denial resolution processes.
- The system extracts billable services from clinical documentation.
- The system enhances documentation precision.
- The system decreases both lost revenue opportunities and denial rates.
Specialty Practices (Cardiology, Orthopaedics, Oncology)
Within specialty practices that face complex coding rules, there is a higher risk of payment denials. AI maintains steady coding procedures while enabling human evaluators to handle difficult situations.
- The system enforces uniform coding standards throughout its operations.
- The system enables evaluators to assess intricate situations.
- The system acquires knowledge through specialized data sets from various fields.
Radiology and Diagnostic Services
Radiology’s structured reporting, combined with repeatable procedures, creates an environment well-suited for automation systems to thrive effectively. AI conducts standard examination tasks while directing the assessment of uncommon situations.
- The system automatically generates medical codes for standard patient appointments.
- The system identifies uncommon situations that need thorough assessment.
- The system enhances operational efficiency while driving revenue growth.
Hospital Inpatient Coding
Hospital inpatient coding is challenging due to extensive records containing multiple diagnoses and conditions. AI extracts relevant information from medical documents to assist coders by working together with electronic health record systems.
- The system displays important medical conditions and their corresponding codes.
- The system arranges intricate medical records.
- The system assists coders during their work within electronic health record systems.
Key Factors to Consider When Selecting AI Medical Coding Services
Choosing a medical coding service is not just a tech choice but an operational one affecting coding, compliance, and revenue. The right healthcare software makes work easier, not more complex. Here are the most important factors healthcare providers should look at before moving forward.
Compatibility with Existing EHR Systems
The proposed solution should work seamlessly with existing Electronic Health Record (EHR) and ERP Systems, ensuring that clinical documentation and coding processes operate within a unified workflow. The system integration process establishes a direct data flow, which helps coding teams to work more efficiently without needing to switch between different tools.
Healthcare-Specific Design
The system needs to verify its operational capacity for real healthcare facilities. The real-world clinical workflows require different automation tools because they possess specific design constraints. A healthcare-oriented system comprehends medical terminology, documentation standards, and payer regulations, thereby providing reliable support for medical billing and coding operations.
Accuracy and Human Oversight
Ensuring accuracy in medical coding is essential to maintain its integrity. Human coders receive assistance from automation, which should function as their supportive tool. The solution allows users to view code suggestions, which can be changed and require final authorization from certified personnel.
HIPAA Compliance and Data Security
Protecting patient information remains a critical requirement in healthcare operations. HIPAA-compliant data management solutions utilize controlled access systems and detailed audit tracing to protect against security threats while meeting industry regulations.
Scalability for Volume and Complexity
As organizations grow, both documentation complexity and coding volume naturally increase. Scalable platforms provide organizations with the ability to handle increased workloads while supporting multiple specialties and their changing business needs without interrupting their existing operational procedures.
Support for Revenue Cycle Objectives
Automation in coding must contribute directly toward achieving revenue cycle goals. The solution generates strategic business value because it decreases claim rejections and improves billing accuracy while shortening the reimbursement process.
Provider Support and Expertise
Effective implementation goes beyond technology alone. The provider needs to deliver complete implementation support, which includes user training, workflow optimization, and ongoing performance enhancement programs that will maintain operational efficiency.
Unsure Which AI Medical Coding Services to Choose?
Get Expert Advice!
The Future of Medical Coding with AI
Healthcare coding is growing more complex due to rising patient numbers, expanded clinical documentation, and the demand for faster work from teams that must avoid mistakes. Intelligent automation supports this shift by handling routine tasks while keeping human expertise central to the process.
Over time, automated solutions manage repetitive cases, allowing experienced coders to focus on complex reviews, audits, and edge cases. This balanced approach improves sustainability and reduces burnout without compromising accuracy or control.
TechnoBrains, a leading healthcare software development company, helps healthcare organizations adopt scalable, compliant coding solutions that fit real workflows and support long-term operational efficiency.
Frequently Asked Questions: AI Medical Coding
AI helps medical coders by reviewing clinical documentation and suggesting accurate codes. It reduces repetitive work, flags missing information, and helps prevent errors before claims are submitted.
AI technology supports medical coders by handling their routine work, while human coders deal with difficult situations which need their special skills.
The right solution depends on factors such as specialty, coding volume, EHR systems, and compliance requirements. Most providers choose AI that fits their workflows and allows human review.
The system’s accuracy improves continuously because it learns from past information and user inputs, but it needs human judgment to assess complicated situations and maintain compliance with regulations.
In today’s healthcare landscape, intelligent coding solutions help organizations improve revenue cycle management because they decrease coding errors and denial rates while they accelerate billing processes and enhancing cash flow.
Yes, many healthcare organizations employ advanced coding technologies as their primary documentation solution, together with human coders.